What steps are you taking to improve indoor air quality and keep your occupants safe?
Recent research shows the virus that causes COVID-19 can survive in the air for much longer than other viruses, remaining infectious for up to 16 hours.
We already know larger droplets such as those from a cough or sneeze are a key method of virus transmission, but normal breathing and speaking still create tiny aerosol particles that remain in the air.
The CDC has also recently updated its guidance to include airborne transmission as a mode of transmission of this virus when in enclosed spaces with inadequate ventilation or air handling.
When we know how easily viruses are spread in public spaces, are there steps that hospitals, schools, offices, and other densely populated buildings should be taking to protect public health?
We spoke with CCG’s UAE Head of MEP Nasser G. Nasser to get his overview and advice on the different methods of air filtration and how to protect the occupants of your building through enhancing indoor air quality.
What does the research show?
Researchers from Tulane University investigated the durability of the tiny aerosol particles and how infectious they remain in the air. It was discovered that the SARS-CoV-2 particles that cause COVID-19 remain infectious for 16 hours with very little deterioration. This makes this strain an anomaly, as other types of coronaviruses deteriorate over this time.
It is important to interpret these results carefully as this was conducted in an artificial laboratory, and isn’t entirely reflective of how the particles would behave in real life settings. Currently, the World Health Organization considers droplet transmission of SARS-CoV-2 as a dominant mode of transmission but does not consider airborne transmission to be one except in specific settings related to healthcare procedures.
However, the US Centers for Disease Control and Prevention (CDC) has recently updated its guidance to include airborne transmission as one of the modes of transmission of this virus in certain circumstances such as in enclosed spaces, through prolonged exposure to respiratory particles or resulting from inadequate ventilation or air handling.
All of this clearly underscores the importance of adequate ventilation and air handling.
What can be done to reduce the spread of airborne viruses in indoor environments?
The virus is most commonly spread through larger droplets, for which the most effective prevention is social distancing, safe hygiene practices and Personal Protective Equipment (PPE). However, transmission of SARS-CoV-2 through the air is sufficiently likely that airborne exposure to the virus should be controlled. Changes to the operation of heating, ventilating, and air-conditioning systems can reduce airborne exposure.
Ventilation and filtration provided by heating, ventilating, and air-conditioning systems can reduce the airborne concentration of SARS-CoV-2 and thus reduce risk of transmission through the air. However, disabling these systems is not generally a recommended measure to reduce virus transmission because unconditioned spaces can cause thermal stress to people that may be directly life threatening and might also lower resistance to infection.
There are various methods of air treatment that have been or are being developed that can either remove or deactivate infectious particles.
Increased ventilation rate
Ventilation is the supply of outdoor air to a building. The higher the ventilation rate, the more frequent the exchange of air is. This helps dilute pathogens and reduce exposure to contaminated air, but increases running costs. Ventilation standards such as ASHRAE 62.1 (published by the American Society for Heating, Refrigeration & Air-Conditioning Engineers) attempt to strike a balance between indoor air quality and energy consumption. Nevertheless, it is recommended to increase fresh air supply and reduce air recirculation as much as possible when the building is operating under adverse conditions such as an airborne pandemic. Ventilation rates vary depending on the building, indoor environment and occupants, but increased rates are usually associated with fewer adverse health effects. Ventilation rates can be increased naturally through windows or doors or mechanically by fans and air handling units.

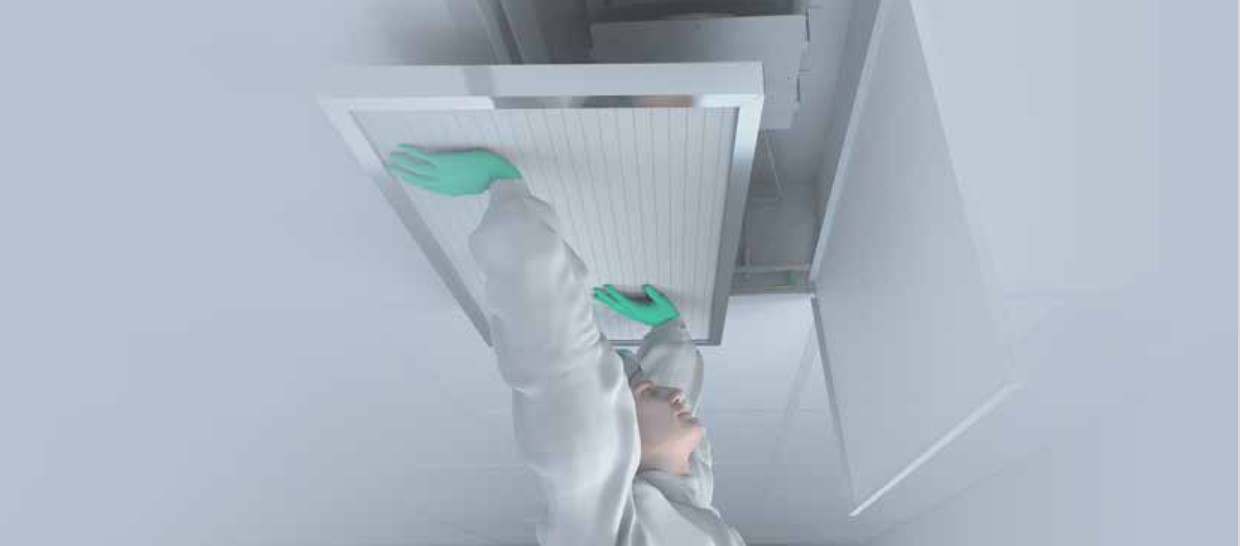
ePM1 filters
While these air filters are not designed specifically to prevent the spread of airborne viruses, their high filtration efficiency reduces the risk. They are considered as first line to reducing the risk of transmission of airborne diseases through HVAC systems. This is because viruses usually attach to airborne particulate matter and aerosols, which this filter removes from the air.

HEPA (High Efficiency Particulate Air) filters
These filters remove pathogens and are considered vital in critical environments within hospitals and healthcare facilities. Since particles are trapped rather than deactivated, the filters must be treated and disposed of as biohazardous waste, using appropriate PPE.
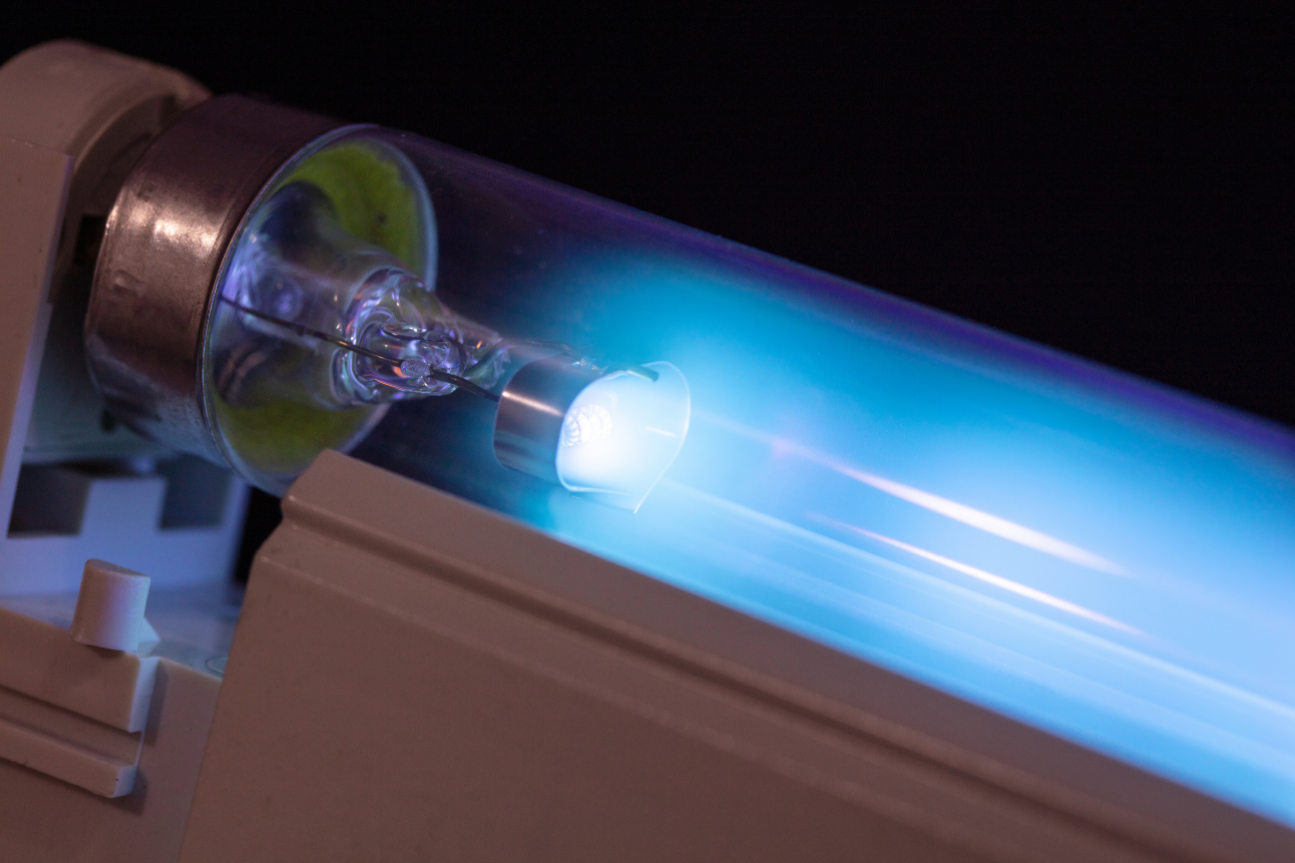
UV disinfection
UV germicidal irradiation reduces transmission of airborne viruses and infections by using short-wave ultraviolet (UV-C) light to deactivate pathogens and microorganisms including mold, bacteria and viruses. UV-C works to sterilize the air by damaging the DNA and RNA of airborne pathogens, rendering them harmless. They can be used as stand-alone devices or installed into HVAC systems. They are commonly used alongside HEPA air filtration as complementary systems for disinfecting high-risk areas of hospitals. Recent research showed UV-C light sources effectively deactivate SARS-CoV-2 and a 5mJ/cm2 dose reduces the virus by 99% in 6 seconds. It is worth mentioning that direct exposure to UV rays can be detrimental to human health.
Bipolar Ionization
Bipolar Ionization was introduced in the 1970s to control pathogens in food manufacturing, and was effective during previous outbreaks of SARS, norovirus and more recently, MERS virus. The technology takes in air molecules and turns them into bipolar charged atoms (positive & negative ions) before releasing them. These ions attach to and deactivate viruses, bacteria, mold, and allergens, by producing a chemical reaction. They also increase their size and mass, which causes them to drop to the floor or to get caught by the filter. It works as an active process, continuously disinfecting air and significantly reducing microbes in a short time. Many hospitals and public buildings employ this method, and its main advantage is the ease of retrofitting it into existing HVAC systems.
Which systems are implemented in hospitals?
Currently, hospitals use central ePM1 filters, central and terminal HEPA filtration systems, UV disinfection and they apply higher ventilation rates compared to non-healthcare buildings. Some hospitals also utilize bi-polar ionization. HEPA filtration is mainly focused on critical spaces where patients are at high-risk, such as operating and isolation rooms, or where processes requiring clean environments are carried out such as sterile IV preparation. In the Middle East, general patient care spaces commonly do not employ systems or technologies specifically designed for removing or eliminating pathogens, but that is changing in newer facilities.
Which systems are used in other buildings?
In the vast majority of non-medical buildings, nothing is used that is capable of removing or eliminating pathogens. Some buildings employ ePM1 filters and a smaller portion employ bipolar ionization. Most rely mainly on ventilation to dilute airborne pathogens, although this cannot happen fast enough to prevent spread through HVAC systems in an airborne pandemic situation such as SARS-CoV-2, and especially not in high density occupancies.
What are the regulations governing air filtration in densely populated spaces during an airborne pandemic?
Currently, there aren’t any. However, guidance and advice has been issued by ASHRAE, CIBSE and REHVA. These organizations provide up-to-date information on how to operate and use building services to minimize virus spread through HVAC and plumbing systems. Governmental and national public health institutions should be consulted for each country to confirm regulations.
Will there be regulations, or will more buildings implement these systems as a result of the pandemic?
CCG’s MEP Manager, Nasser, personally believes there should be changes made to the current codes, standards and regulations as a result of the pandemic, especially since scientists believe pandemics will become more common.
Following the guidance from ASHRAE, CIBSE and REHVA, building readiness plans, assessments and systems evaluations should be incorporated into future editions of codes and standards.
Furthermore, changes should be introduced to ventilation design such as including an in-built pandemic operation mode in the controls where more outdoor air is introduced, higher efficiency filters temporarily replace standard filters and fan speeds are ramped up to overcome the resistance from these filters. Alternatively, a general increase in the fresh air requirements and filtration efficiency under normal operation may be considered.
Limitations on the sizes of zones sharing HVAC equipment might be enforced in new buildings to limit the spread of pathogens. However, it is not sustainable for HEPA filters or UV disinfection to be broadly implemented, due to the high capital and operational costs and consequent environmental impact.
What is your advice for current and new buildings?
Governmental and national public health institutions should be consulted in each country, to confirm regulations for businesses and public spaces. Follow the advice issued by ASHRAE, CIBSE and REHVA, create a building readiness plan and conduct a systems evaluation to maintain high indoor air quality and minimize occupants’ exposure to airborne virus particles. The potential benefit to public health during this pandemic will outweigh the temporary reduction in energy efficiency that comes as a result of these measures.

Nasser G. Nasser has over 14 years of experience in building services covering all aspects of MEP design, construction and project management from inception through to completion and beyond. His areas of expertise include healthcare facilities, high-rise towers, hospitality and residential buildings and more. He is a member of the Chartered Institute of Building Services Engineers, an AEE Certified Energy Manager and a NFPA Certified Fire Protection Specialist. He designed several healthcare facilities throughout the Middle East and in 2016, he led the mechanical services design for Sheikh Khalifah Central Hospital in Fujairah, UAE where he implemented all of the technologies mentioned in this article. The project is in the final stages of construction and is under CCG’s supervision.




